How to Prevent a Deadly Ruptured Aorta
 Actor Alan Thicke died earlier this week of a ruptured aorta – about three hours after it first developed a tear.
Actor Alan Thicke died earlier this week of a ruptured aorta – about three hours after it first developed a tear.
An aortic tear also killed actor and comedian John Ritter in 2003.
But the first time I heard of this happening was when it happened to someone I knew personally – my mom had a violin student, Brian, who was in his 40s. He had to stop taking lessons with her for a while, after experiencing this medical emergency. At the time he told us it was quite rare. Fortunately he quickly got emergency treatment and made an excellent recovery.
Like both of these actors, Brian was in good health leading up to their deaths.
So what exactly is a ruptured aorta, how does it happen, and is there anything you can do to prevent it from happening?
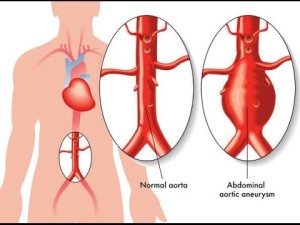
The aorta is the main artery that carries blood from the heart to other parts of the body. This condition strikes approximatley 10,000 Americans a year.
According to MedicineNet, Aortic dissection occurs when a tear occurs in the inner muscle wall lining of the aorta, allowing blood to split apart the muscle layers of the aortic wall. Symptoms of aortic dissection include a tearing or ripping pain in the chest, sweating, nausea, shortness of breath, weakness, or fainting.
According to Dr. GORDON EWY (Director, University of Arizona Sarver Heart Center), there are certain inherited conditions that weaken the aorta, and it runs in families. Conditions like atherosclerosis or high blood pressure can also contribute to it.
From the Health Communities website:
The exact cause for aortic dissection is unknown; however, risk factors associated with the condition have been identified. High blood pressure (hypertension) is the leading risk factor. Hypertension, which is present in 2/3 of all cases, puts pressure on the aortic wall, weakening it and making it more likely to tear.
Other risk factors include the following:
- Aortic aneurysm (enlarged blood vessel)
- Aortic valve problems (e.g., aortic stenosis)
- Cocaine use
- Connective tissue disorders (e.g., scleroderma)
- Family history of aortic dissection
- Hardening of the arteries (atherosclerosis)
- Narrowing or enlargement of the aorta
- Syphilis (sexually transmitted disease [STD] caused by bacteria)
Genetic (hereditary) connective tissue disorders can increase the risk for aortic dissection. Patients who have Marfan syndrome or Ehlers-Danlos syndrome (conditions that weaken connective tissue) are at increased risk for blood vessel rupture. Turner syndrome, which occurs in patients who have 45 chromosomes instead of the normal 46, can lead to heart problems and high blood pressure, increasing risk for aortic dissection.
Blunt trauma to the chest (in a car accident, for example) is another potential cause for aortic dissection.
BottomLine Heath tells us how to prevent this deadly emergency:
The rate of survival from this condition increases dramatically when patients with a partial aortic dissection, which can lead to an aortic rupture, recognize the symptoms and get to an emergency room immediately. Often it’s possible to prevent an aortic dissection altogether by getting a screening test to diagnose arterial weakness before there’s an emergency.
What you need to know to save your life—or that of a loved one…
Every drop of blood in the body passes through the aorta. About the diameter of a garden hose, the aorta originates in the left ventricle of the heart, rises into the chest and then descends into the abdomen.
Most aortic dissections occur in a damaged section of artery known as an aneurysm—this balloonlike bulge thins and weakens that area of the artery. Within this area, a small tear can form in the inner layer (tunica intima) of the blood vessel, creating a dissection.
What happens: Blood forces its way into the tear, widening it and eventually separating, or dissecting, the three layers of the blood vessel. The continued force of blood cuts through the arterial layers and creates a “false channel,” or lumen. Patients can survive this initial dissection—in some cases, they won’t even know that anything is wrong if the damage stops there. But often it doesn’t.
Without treatment, 15% to 20% of patients with an aortic dissection will suffer (usually within minutes or days) an acute rupture, in which the aorta is completely torn. When this happens, liters of blood are lost within a minute, and many victims die within seconds. Many others with an untreated aortic dissection suffer a rupture at some later date.
TELLTALE SYMPTOMS
The symptoms of an aortic dissection can mimic those of a heart attack. Most patients with an aortic dissection experience sudden pain that’s centered in the chest, but pain can also occur in the back or neck. They often describe the pain as a brief “ripping” sensation.
Other symptoms may include nausea, shortness of breath or heavy sweating. Victims may suffer a precipitous drop in blood pressure from inadequate circulation, causing light-headedness or fainting.
Some people with aortic dissection experience only vague discomfort, similar to indigestion. In rare cases, an aortic dissection may cause no symptoms and be discovered during an imaging test for some other medical condition.
Typically, however, an aortic dissection is diagnosed after the patient complains of symptoms and receives a CT or MRI scan or a transesophageal echocardiogram, in which an ultrasound device is inserted into the throat to create an image of the heart’s valves and chambers. An aortic dissection cannot be ruled out with a chest X-ray or an electrocardiogram, which records the heart’s electrical activity and is often used to diagnose a heart attack.
EMERGENCY REPAIR IS CRITICAL
When an aortic dissection is detected, emergency surgery is always recommended, unless the patient is too frail to undergo an operation.
About 50% of dissections occur in the ascending aorta (in the chest) and these almost always require…
advertisement
- Open surgery, which involves opening the chest and cutting out the damaged section of artery and replacing it with a synthetic tube. It’s a complicated procedure, but more than 90% of patients will survive when it’s done by an experienced doctor, assuming that the patients get to the operating room in time.
Most of the other dissections occur in the descending portion of the aorta (in the abdomen) and are usually treated with…
- Endovascular stents that restore normal blood flow. Rather than cutting out the damaged section of artery with an open procedure, a catheter is inserted through a blood vessel in the groin and threaded upward into the damaged area. Then a fabric tube reinforced with metal stents (also known as a scaffold) is used to restore the circulation pathway.
This procedure is preferred, in appropriate cases, because patients recover more quickly and have a lower risk for kidney damage and neurological complications than those who undergo open surgery.
Important finding: A three-year study that looked at the medical records of 28,000 patients found that the risk of dying in the hospital following an endovascular repair of a rupture in the descending aorta was 1.9%, compared with 5.2% following open surgery.
Patients who can’t undergo surgery, often due to other medical problems, may be treated with analgesics and medications that lower blood pressure and reduce the risk that a dissection will worsen. Blood pressure should be routinely monitored and a CT or MRI scan performed every six to 12 months.
BEST APPROACH: PREVENTION
Because aortic dissections almost always occur within aneurysms, detecting the bulging artery is the first step in prevention. This can be tricky because aneurysms typically cause no symptoms until a dissection—or a complete rupture—occurs. Important…
- Get screened. I advise everyone to have an ultrasound starting at age 60—or, in some cases, an MRI or contrast CT scan—to screen for aortic aneurysms. Earlier screening is typically recommended if you have a family history of aneurysm or aortic dissection.
Screening is crucial for men with a history of smoking. Men are twice as likely as women to have an aortic dissection, and smoking doubles the risk once again. Screening is also important for women if they have smoked or have a history of heart disease, or a family history of aneurysm or aortic dissection.
Patients with no sign of disease usually don’t require additional tests/screening. However, high-risk patients, such as those with a family history of aneurysm or aortic dissection, should get retested at least every five years—more often if they already have an aneurysm.
- Earlier treatment. Aortic aneurysms usually grow slowly, at the rate of about 1/100 of an inch in diameter annually. Because smaller aneurysms may never grow to a size that will cause a serious risk, we currently don’t advise surgery or stenting until an aneurysm reaches about two inches in diameter.
However, having the procedure done at the time of diagnosis is the safest choice for those who are most likely to suffer an aortic rupture—people with uncontrolled hypertension… a family history of aortic dissection or aortic aneurysm… or a genetic condition called Marfan syndrome, which weakens the artery wall.
- Blood pressure control. Along with not smoking, controlling blood pressure is the best way to prevent aortic dissection, since most cases occur in patients with hypertension. Keep your blood pressure under 120/80.
- Risk factor sometimes overlooked: High cholesterol. Aortic aneurysms and dissections usually occur in people with atherosclerosis, the accumulation of fatty deposits that weaken the artery walls. Maintaining healthy cholesterol is among the best ways to prevent this.






Leave a Reply